LEPROSY
AN INFECTIOUS DISEASE CAUSES BY : MYCOBACTERIUM LEPRAE
Leprosy is an infectious disease that causes severe, disfiguring skin sores and nerve damage in the arms, legs, and skin areas around the body. The disease has been around since ancient times, often surrounded by terrifying, negative stigmas and tales of leprosy patients being shunned as outcasts. Outbreaks of leprosy have affected, and panicked, people on every continent. The oldest civilizations of China, Egypt, and India feared leprosy was an incurable, mutilating, and contagious disease. However, leprosy is actually not that contagious. You can catch it only if you come into close and repeated contact with nose and mouth droplets from someone with untreated leprosy. Children are more likely to get leprosy than adults.
Today, about 180,000 people worldwide are infected with leprosy, according to the World Health Organization, most of them in Africa and Asia. About 100 people are diagnosed with leprosy in the U.S. every year, mostly in the South, California, Hawaii, and some U.S. territories.




WHAT CAUSES LEPROSY?
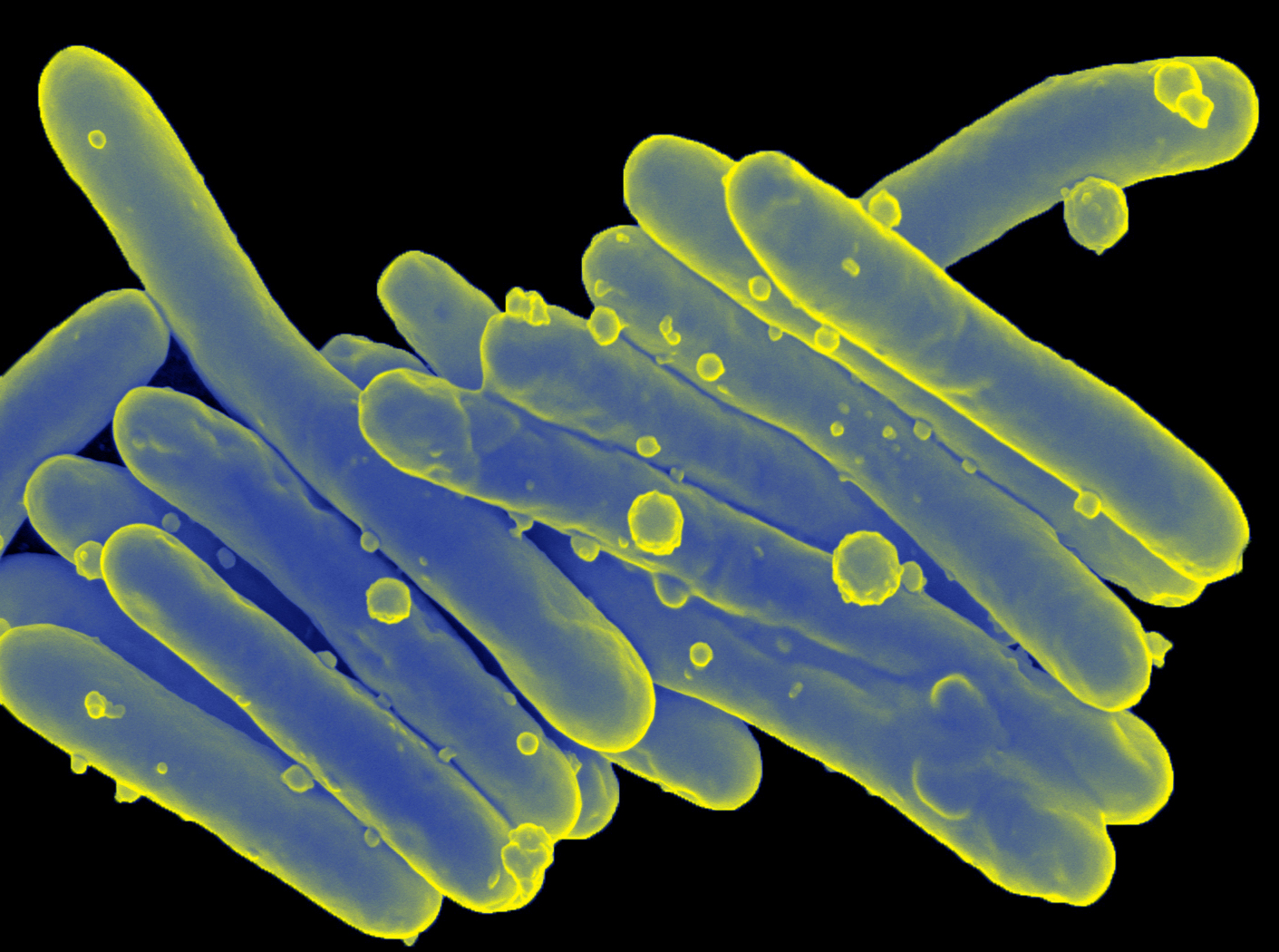
Leprosy is caused by a slow-growing type of bacteria called Mycobacterium leprae (M. leprae). Leprosy is also known as Hansen's disease, after the scientist who discovered M. leprae in 1873.
WHAT ARE THE SYMPTOMS OF LEPROSY?
Leprosy primarily affects the skin and the nerves outside the brain and spinal cord, called the peripheral nerves. It may also strike the eyes and the thin tissue lining the inside of the nose. The main symptom of leprosy is disfiguring skin sores, lumps, or bumps that do not go away after several weeks or months. The skin sores are pale-colored.
Nerve damage can lead to:
1. Loss of feeling in the arms and legs
2. Muscle weakness
It usually takes about 3 to 5 years for symptoms to appear after coming into contact with the leprosy-causing bacteria. Some people do not develop symptoms until 20 years later. The time between contact with the bacteria and the appearance of symptoms is called the incubation period. Leprosy's long incubation period makes it very difficult for doctors to determine when and where a person with leprosy got infected.
FORMS OF LEPROSY
Leprosy primarily affects the skin and the nerves outside the brain and spinal cord, called the peripheral nerves. It may also strike the eyes and the thin tissue lining the inside of the nose. The main symptom of leprosy is disfiguring skin sores, lumps, or bumps that do not go away after several weeks or months. The skin sores are pale-colored.
Tuberculoid :A mild, less severe form of leprosy. People with this type have only one or a few patches of flat, pale-colored skin (paucibacillary leprosy). The affected area of skin may feel numb because of nerve damage underneath. Tuberculoid leprosy is less contagious than other forms.
Lepromatous : A more severe form of the disease. It has widespread skin bumps and rashes (multibacillary leprosy), numbness, and muscle weakness. The nose, kidneys, and male reproductive organs may also be affected. It is more contagious than tuberculoid leprosy.
Borderline : People with this type of leprosy have symptoms of both the tuberculoid and lepromatous forms.
HOW IS LEPROSY DIAGNOSED?
If you have a suspicious skin sore, your doctor will remove a small sample of the abnormal skin and send it to a lab to be examined. This is called a skin biopsy. A skin smear test may also be done. With paucibacillary leprosy, no bacteria will be detected. In contrast, bacteria are expected to be found on a skin smear test from a person with multibacillary leprosy.
HOW IS LEPROSY TREATED?
Leprosy can be cured. In the last two decades, 16 million people with leprosy have been cured. The World Health Organization provides free treatment for all people with leprosy. Treatment depends on the type of leprosy that you have. Antibiotics are used to treat the infection. Long-term treatment with two or more antibiotics is recommended, usually from six months to a year. People with severe leprosy may need to take antibiotics longer. Antibiotics cannot treat the nerve damage. Anti-inflammatory drugs are used to control nerve pain and damage related to leprosy. This may include steroids, such as prednisone. Patients with leprosy may also be given thalidomide, a potent medication that suppresses the body's immune system. It helps treat leprosy skin nodules. Thalidomide is known to cause severe, life-threatening birth defects and should never be taken by women who are pregnant or women who may become pregnant.
LEPROSY COMPLICATIONS
Without treatment, leprosy can permanently damage your skin, nerves, arms, legs, feet, and eyes.
Complications of leprosy can include :
> Blindness or glaucoma
> Disfiguration of the face (including permanent swelling, bumps, and lumps)
> Erectile dysfunction and infertility in men
> Kidney failure
> Muscle weakness that leads to claw-like hands or an inability to flex the feet
> Permanent damage to the inside of the nose, which can lead to nosebleeds and a chronic, stuffy nose
> Permanent damage to the nerves outside the brain and spinal cord, including those in the arms, legs, and feet
Nerve damage can lead to a dangerous loss of feeling. A person with leprosy-related nerve damage may not feel pain when the hands, legs, or feet are cut, burned, or otherwise injured.
ORIGIN OF LEPROSY
Leprosy, a chronic human disease with potentially debilitating neurological consequences, results from infection with Mycobacterium leprae. This unculturable pathogen has undergone extensive reductive evolution, with half of its genome now occupied by pseudogenes. Using comparative genomics, we demonstrated that all extant cases of leprosy are attributable to a single clone whose dissemination worldwide can be retraced from analysis of very rare single-nucleotide polymorphisms. The disease seems to have originated in Eastern Africa or the Near East and spread with successive human migrations. Europeans or North Africans introduced leprosy into West Africa and the Americas within the past 500 years.
HISTORY OF LEPROSY TREATMENT : THE LONG FIGHT IS NOT OVER YET
1873: Dr. Armauer Hansen of Norway was the first to see the leprosy germ under a microscope. This was a revolutionary discovery. The evidence was clear: leprosy is caused by a germ (Mycobacterium leprae). It was not hereditary, a curse, or from sin. Because of Dr. Hansen's work, leprosy is also called Hansen's disease.
1894: "Carville" is established as a state leprosy hospital in Carville, Louisiana.
Early 20th century: From the early 1900s through the late 1940s, leprosy doctors in Africa, Asia, the Far East, South America and elsewhere injected patients with oil from the chaulmoogra nut. This painful treatment appeared to work for some patients. Long term benefits were questionable, though.
1906: The organization that would become American Leprosy Missions is founded in New York City by a group of seven prominent ministers, mission executives and businessmen at the urging of Thomas Bailey, a representative from the London-based "Mission to Lepers in India and the East".
1941: This year saw the introduction of promin for leprosy treatment at "Carville," the U.S. Public Health Service facility in Louisiana. There was a painful downside to promin: it required too many injections.
1950s: Dr. R.G. Cochrane was a pioneer in the use of dapsone pills which became the treatment of choice during the 1950s. Disappointment followed, though, as the leprosy bacilli began developing dapsone resistance. The germs were becoming smarter than the medicine.
1970s: Success at last! Drug trials on the island of Malta in the 1970s led to an effective combination of drugs to treat leprosy.
1981: The World Health Organization started recommending multi-drug therapy, or MDT. The three drugs, taken in combination, are dapsone, rifampicin (or rifampin) and clofazimine. Treatment takes from six months to a year or more.
1982: American Leprosy Missions began using multi-drug therapy in its projects. During the last 18 years, millions of people have been cured of leprosy with MDT.
2011: Early treatment with MDT is the best prevention against nerve damage and deformities. There is still no vaccine against leprosy, although American Leprosy Missions has been funding vaccine research.
LEPROSY VACCINE
Since 2002, American Leprosy Missions has been committed to working towards the development of the world's first leprosy vaccine and a new leprosy diagnostic test in partnership with the non-profit Infectious Disease Research Institute (IDRI) in Seattle, Washington. During the past ten years we have invested almost $4 million into developing the vaccine and diagnostic test.
WHY IS A LEPROSY VACCINE NEEDED?
Leprosy remains one of the most dreaded diseases in the world, a disease that isolates and shames its victims. Active leprosy cases and leprosy-related disabilities affect more than 4 million people in the world today. Immunizations are the most cost-effective way to eliminate disease.
In late October 2011, more than 20 scientists and global health experts gathered at Emory University's Rollins School of Public Health to discuss the current leprosy vaccine research. Read more. In 2013, vaccine toxicology studies will take place, with safety trials starting in 2014.
WHAT COULD BE THE IMPACT OF A NEW DIAGNOSTIC TEST?
Leprosy diagnosis currently requires a well-trained clinician who can recognize the symptoms. This can be impossible in poor, remote areas. A new, easy-to-administer diagnostic test can detect the bacteria before symptoms appear, enabling treatment to be administered before the disease has irreparably damaged nerves.
In early 2013, IDRI announced that a new, rapid diagnostic test for leprosy was registered for use in Brazil. According to Malcolm Duthie, Senior Scientist at IDRI, the diagnostic test is simple, easy to use and accurate. "You add a drop of blood and a couple of drops of a developing reagent to the test and a line develops," he explained. "From there, it's somewhat like a pregnancy test: the appearance of two lines indicate the test is positive and the person has leprosy."
